Pain is a Global Problem
Over 1.5 billion people worldwide suffer from chronic pain.1 Nearly one third of American adults experience chronic pain,2 and almost one in five surveyed Europeans indicated they have moderate or severe chronic pain3 The three most common sources of chronic pain are low back pain (29%), neck pain (16%), and severe headache or migraine pain (15%).4
PAIN CAN BE ACUTE OR CHRONIC
Acute pain warns you that you have been hurt. It starts suddenly, and when the injury heals, the pain stops. In acute injury, the pain is due to pressure from inflammation in the tissues and nerves at the site of the injury. This inflammation leads to the swelling that is observable and is part of the body’s healing response.
Chronic pain continues after the injury has healed, lasting for weeks, months, even years. In chronic injury, nerve signals that were active during acute injury continue to send messages that the body is in pain. Although chronic pain is not completely understood, it is potentially due to nerves that have become damaged. New research also suggests that chronic pain can come from a malfunction in the way the brain ‘maps’ sensory information.5
PAIN AND QUALITY OF LIFE
Nearly two-thirds of people with chronic pain report problems sleeping. Lack of restorative sleep often makes the pain worse, thus resulting in a frustrating cycle of pain and sleeplessness. Unrelieved pain can result in longer hospital stays, increased re-hospitalizations, increased outpatient visits, and decreased ability to function, leading to lost income and insurance coverage. In addition to the financial burden that comes with chronic pain, the emotional costs to patients and family can be high as well.
Chronic pain constitutes a tremendous expense to employers in healthcare and rehabilitation costs, and lost worker productivity. Migraine is the 3rd most prevalent disease on the planet6 and a 2015 study showed that headache pain was the most commonly attributed cause of lost productive time at work in the U.S.7
DRUGS ARE NOT THE ANSWER
Drugs are often prescribed to deal with a patient’s pain as a first line treatment. Yet only 23% of patients with chronic pain found opiates effective, according to a 2006 survey by the American Pain Foundation8 and a recent review found that opioids at guideline recommended doses were not effective for low back pain.9 The first randomized study to ever evaluate the long-term effectiveness of opioid for pain relief found that those taking opioids were actually in more pain at 12-months compared to those who were on non-opioid pain relief.10 Opiate abuse and depression have become common in the pain equation and in the United States, and prescription opiates result in more deaths due to overdose than heroin.11 An estimated two million individuals in the United States are addicted to prescription opioids, resulting in an economic cost of $78.5 billion USD annually12
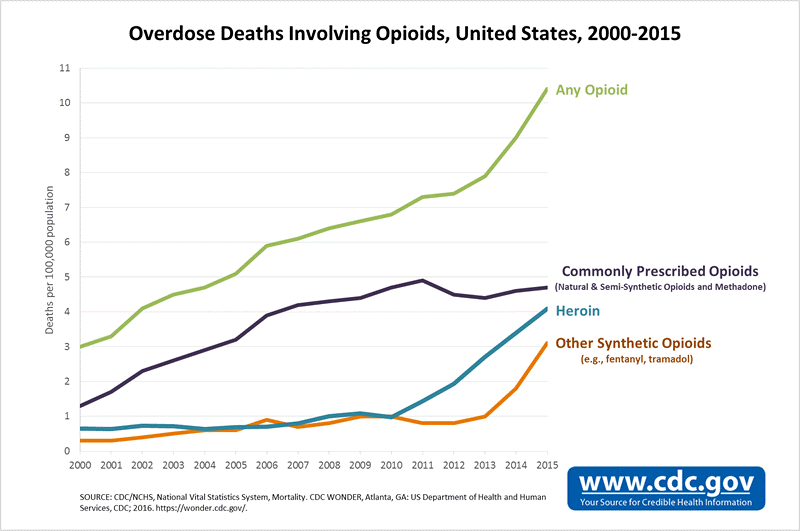
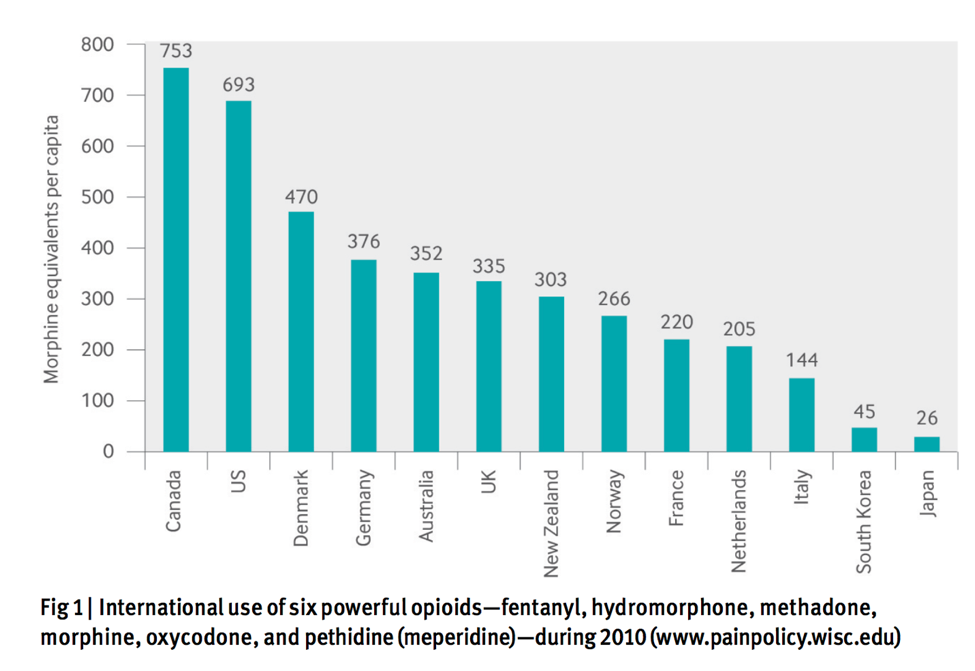
While the dangers and negative effects of prescription opioids have received the most attention in the United States, new data indicates that this is a growing problem worldwide, with significant consumption in many European countries as well as Australia and New Zealand.13
Non-steroidal anti-inflammatory drugs (NSAIDs), the most commonly used medications in the world,14 are another commonly prescribed first-line treatment for pain. However, a recent study of over 440,000 patients found that using any NSAID, including over the counter drugs like Ibuprofen, for even a short period of time was associated with an increased risk of acute heart attack, even in healthy people.15 In the UK, the annual cost of treating gastrointestinal harms caused by NSAID’s was £166-£367 million per year in 1999 and the number of patients on these has stayed the same, at around 7.5% of the overall population.16
ACUPUNCTURE IS EXCELLENT FOR PAIN
Acupuncture is widely known for its effectiveness in the treatment of pain. Its unique role in reducing suffering in patients experiencing pain is one of the main reasons it has become so popular around the world. The research is plentiful on the effects of acupuncture on specific painful conditions, as can be seen throughout this website. For acute pain, a systematic review of 13 trials found that acupuncture was more effective than both sham needling and injection with painkillers.18
For chronic pain, in the largest study of its kind to date, 454,920 patients were treated with acupuncture for headache, low back pain, and/or osteoarthritis in an open pragmatic trial. Effectiveness was rated as marked or moderate in 76% of cases by the 8,727 treating physicians.19 In a 2-year retroactive survey of over 89,000 patients published in 2016, 93% of patients said that their acupuncturist had been successful in treating their musculoskeletal pain.20
A meta-analysis of 17,922 patients from randomized trials concluded, “Acupuncture is effective for the treatment of chronic pain and is therefore a reasonable referral option. Significant differences between true and sham acupuncture indicate that acupuncture is more than a placebo.”21 A follow up study with this data looking at long-term pain relief, found that the benefits of acupuncture persisted 12 months after treatment ended.22
Another study in the journal, Current Opinion in Anesthesiology, in the paper titled ‘Acupuncture for Chronic Pain: an Update and Critical Overview’ concluded that “mounting evidence supports the effectiveness of acupuncture to treat chronic low back, neck, shoulder, and knee pain, as well as headaches. Additional data are emerging that support the use of acupuncture as an adjunct or alternative to opioids, and in perioperative settings.”23
HOW ACUPUNCTURE WORKS FOR PAIN
The mechanisms underlying how acupuncture is so effective for treating pain have been researched extensively for over 60 years. While there is still much left to learn about acupuncture mechanisms and the human body in general, the neural pathways from acupuncture point stimulation, to the spinal cord to the deactivation of the pain centers in the brain have been mapped.2425 Acupuncture has been demonstrated to activate a number of the body’s own opioids as well as improving the brain’s sensitivity to opioids.26 A number of other biochemicals involved in pain reduction have been found to be released or regulated by acupuncture stimulation, including ATP and adenosine, GABA and substance P.27
In the context of ineffective and often dangerous pharmaceutical options for pain, acupuncture represents a safe and effective alternative with a long track-record of successful use.
References:
- 1. National Center for Health Statistics (2006) Health, United States, 2006 [Online] Available from: https://www.cdc.gov/nchs/data/hus/hus06.pdf [Accessed 12 Sept 2017].
- 2. Johannes, C. B., Le, T. K., Zhou, X., Johnston, J. A., & Dworkin, R. H. (2010). The prevalence of chronic pain in United States adults: results of an Internet-based survey. The Journal of Pain : Official Journal of the American Pain Society, 11(11), 1230–1239. http://doi.org/10.1016/j.jpain.2010.07.002
- 3. Breivik H, Collett B, Ventafridda V, Cohen R, Gallacher D. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. Eur J Pain. 2006;13:287–333. doi: 10.1016/j.ejpain.2005.06.009.
- 4. National Center for Health Statistics (US. “Health, United States, 2016: with chartbook on Long-term trends in health. Hyattsville, MD. 2017.”
- 5. Moseley, G. L., & Flor, H. (2012). Targeting cortical representations in the treatment of chronic pain: a review. Neurorehabilitation and neural repair, 26(6), 646-652. DOI: 1177/1545968311433209
- 6. Fried, N. T., Elliott, M. B., & Oshinsky, M. L. (2017). The Role of Adenosine Signaling in Headache: A Review. Brain Sciences, 7(3). http://doi.org/10.3390/brainsci7030030
- 7. National Center for Complementary and Integrative Health (2015) NIH Analysis Shows Americans Are In Pain. [Online] Available from: https://nccih.nih.gov/news/press/08112015 [Accessed 12 Sept 2017]
- 8. The CHP Group (2014) The Cost of Chronic Pain:How Complementary and Alternative Medicine Can Provide Relief. [Online] Available from: http://www.chpgroup.com/wp-content/uploads/2014/12/CHP-WP_CAM-Chronic-Pain_Sls_12.12.2014.pdf [Accessed 12 Sept 2017].
- 9. Abdel Shaheed, C., Maher, C. G., Williams, K. A., Day, R., & McLachlan, A. J. (2016). Efficacy, Tolerability, and Dose-Dependent Effects of Opioid Analgesics for Low Back Pain: A Systematic Review and Meta-analysis. JAMA Internal Medicine, 176(7), 958–968. http://doi.org/10.1001/jamainternmed.2016.1251
- 10. Krebs EE. Effectiveness of opioid therapy vs. non-opioid medication therapy for chronic back & osteoarthritis pain over 12 months. Inannual meeting, Society for General Internal Medicine, Washington DC 2017.
- 11. Rudd RA, Seth P, David F, Scholl L. Increases in Drug and Opioid-Involved Overdose Deaths — United States, 2010–2015. MMWR Morb Mortal Wkly Rep 2016;65:1445–1452. DOI: http://dx.doi.org/10.15585/mmwr.mm655051e1
- 12. Schuchat, A., Houry, D., & Guy, G. P. (2017). New Data on Opioid Use and Prescribing in the United States. Jama, 318(5), 425–426. http://doi.org/10.1001/jama.2017.8913
- 13. Deyo, R. A., Korff, Von, M., & Duhrkoop, D. (2015). Opioids for low back pain. BMJ (Clinical Research Ed.), 350, g6380. http://doi.org/10.1136/bmj.g6380
- 14. Motgahre, V. M., Bajait, C. S., & Turankar, A. (2016). Prescription pattern and adverse drug reaction profile of drugs prescribed with focus on NSAIDs for orthopedic indications at a tertiary care hospital. Skin. http://doi.org/10.18231/2393-9087.2016.0007
- 15. Bally, M., Dendukuri, N., Rich, B., Nadeau, L., Helin-Salmivaara, A., Garbe, E., & Brophy, J. M. (2017). Risk of acute myocardial infarction with NSAIDs in real world use: bayesian meta-analysis of individual patient data. BMJ (Clinical Research Ed.), 357, j1909–13. http://doi.org/10.1136/bmj.j1909
- 16. Cai, S., Garcia Rodriguez, L. A., Masso-Gonzalez, E. L., & Hernandez-Diaz, S. (2009). Uncomplicated peptic ulcer in the UK: trends from 1997 to 2005. Alimentary Pharmacology & Therapeutics, 30(10), 1039–1048. http://doi.org/10.1111/j.1365-2036.2009.04131.x
- 17. Bally, M., Dendukuri, N., Rich, B., Nadeau, L., Helin-Salmivaara, A., Garbe, E., & Brophy, J. M. (2017). Risk of acute myocardial infarction with NSAIDs in real world use: bayesian meta-analysis of individual patient data. BMJ (Clinical Research Ed.), 357, j1909–13. http://doi.org/10.1136/bmj.j1909
- 18. Xiang, A., Cheng, K., Xu, P., & Liu, S. (n.d.). The immediate analgesic effect of acupuncture for pain: a systematic review and meta-analysis.
- 19. Weidenhammer W, Streng A, Linde K, Hoppe A, Melchart D. Acupuncture for chronic pain within the research program of 10 German Health Insurance Funds–basic results from an observational study. Complementary therapies in medicine. 2007;15(4):238-46.
- 20. American Specialty Health Incorporated Health Services Department. (2016). Acupuncture: Does Acupuncture Provided Within a Managed Care Setting Meet Patient Expectations and Quality Outcomes?, 1–12.
- 21. Vickers, A. J., Cronin, A. M., Maschino, A. C., Lewith, G., MacPherson, H., Foster, N. E., et al. (2012). Acupuncture for Chronic Pain. Archives of Internal Medicine, 172(19), 1444. http://doi.org/10.1001/archinternmed.2012.3654
- 22. MacPherson, H., Vertosick, E. A., Foster, N. E., Lewith, G., Linde, K., Sherman, K. J., et al. (2016). The persistence of the effects of acupuncture after a course of treatment. Pain, 1–22. http://doi.org/10.1097/j.pain.0000000000000747
- 23. Yin, C., Buchheit, T. E., & Park, J. J. (2017). Acupuncture for chronic pain: an update and critical overview. Current Opinion in Anaesthesiology, 1. http://doi.org/10.1097/ACO.0000000000000501
- 24. Longhurst, J., Chee-Yee, S., & Li, P. (2017). Defining Acupuncture’s Place in Western Medicine. Scientia, 1–5.
- 25. Zhang, Z.-J., Wang, X.-M., & McAlonan, G. M. (2012). Neural Acupuncture Unit: A New Concept for Interpreting Effects and Mechanisms of Acupuncture. Evidence-Based Complementary and Alternative Medicine, 2012(3), 1–23. http://doi.org/10.1016/j.brainresbull.2007.08.003
- 26. Harris, R. E., Zubieta, J.-K., Scott, D. J., Napadow, V., Gracely, R. H., & Clauw, D. J. (2009). Traditional Chinese acupuncture and placebo (sham) acupuncture are differentiated by their effects on μ-opioid receptors (MORs). NeuroImage, 47(3), 1077–1085. http://doi.org/10.1016/j.neuroimage.2009.05.083
- 27. Zhao, Z.-Q. (2008). Neural mechanism underlying acupuncture analgesia. Progress in Neurobiology, 85(4), 355–375. http://doi.org/10.1016/j.pneurobio.2008.05.004



